School of Health Graduate Students’ Approach to Health Care Delivery Informed by Their Diverse Backgrounds
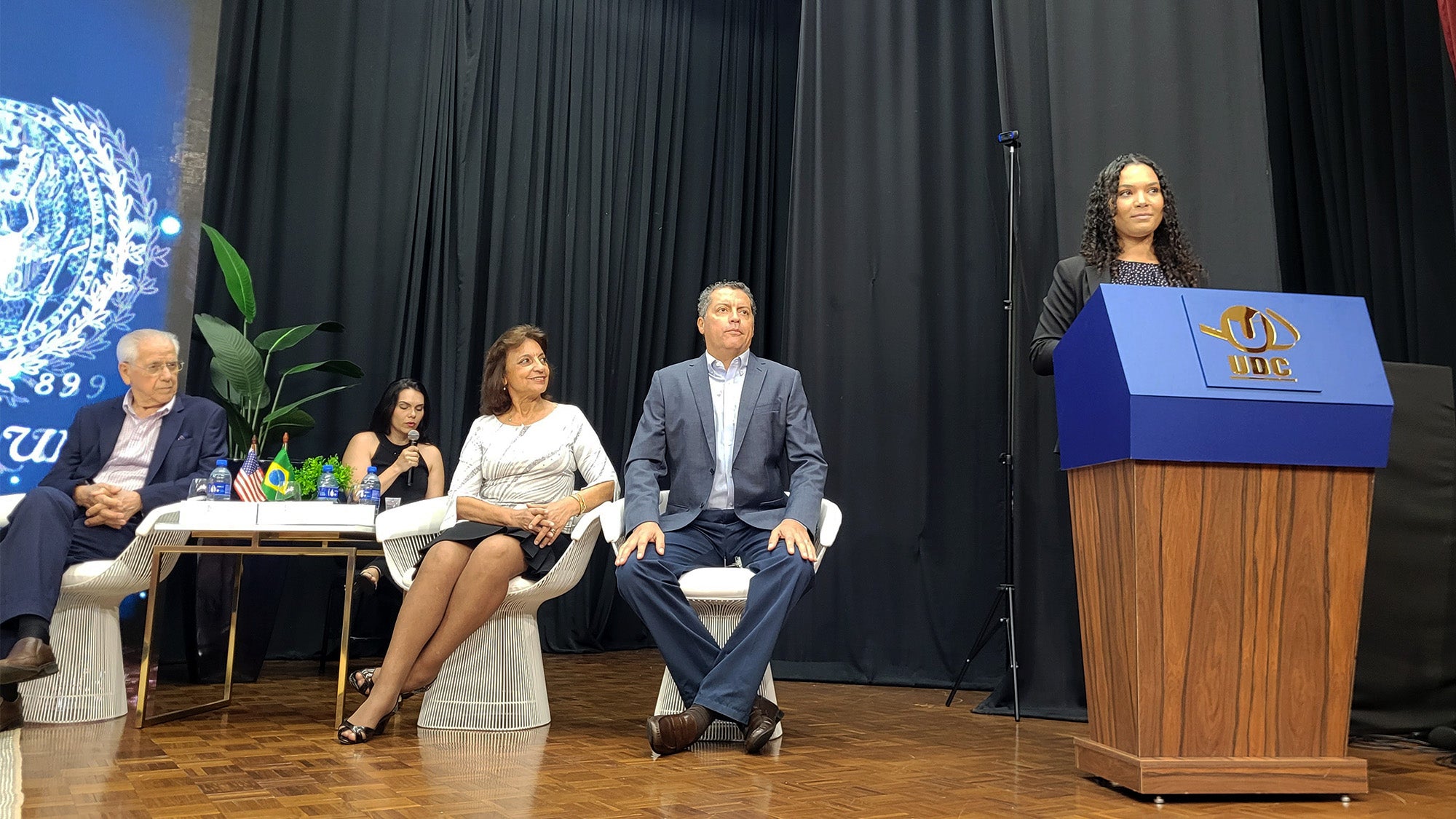
Top Image: In 2023, Jayla Romain (G’24) traveled to Brazil with a group of Master of Science in Health Systems Administration students to study health care systems in the country as part of the comparative health systems global experience offered by the program. On the trip, she addressed students and faculty at Centro Universitário Dinâmica das Cataratas in Foz do Iguaçu, Brazil.
(May 11, 2024) — Graduate students in the next two cohorts of Georgetown’s Master of Science in Health Systems Administration (MHSA) come to the program with diverse working backgrounds in the health care sector — from nursing, law and global health non-governmental organizations (NGOs). Their varied experiences inform their approaches to improving health care delivery.
The two-year graduate program requires incoming students to have full-time work experience of one to five years in the health care sector. Courses cover a range of topics, including financial management, health politics and policy, population health analytics and data visualization. Over spring break, students can participate in an optional comparative health systems global experience, which provides the opportunity to travel to other countries to visit health care delivery sites, engage with health system leaders, and participate in team-based activities. Destinations have included Singapore, Seoul, South Korea and Brazil.
The cohort size of each MHSA class remains small — around a dozen — and upon completion of the program most graduates find employment with hospitals and health systems, although some of the 400 MHSA alumni to date have pursued careers in consulting firms and federal agencies.
Bringing the Voice of Frontline Workers to Hospital Administrative Offices
Jayla Romain (G’24) graduated with her Bachelor of Science in nursing in 2020 as the COVID-19 pandemic took hold. For the past 3 ½ years, she has worked as a bedside nurse at Vanderbilt University Medical Center in Nashville, Tennessee.

Jayla Romain (G’24)
Romain initially thought she would go to graduate school to become a nurse practitioner, but instead chose to pursue her MHSA degree because she felt more people in hospital administrator roles should have frontline health care delivery experience.
“Working beside through COVID was an eye-opening experience, and I noticed a gap between hospital administrators and nurses on the frontline when it came to decisions about care delivery, supply chain questions, and operations,” said Romain. “I want to bridge that gap and use my education to make an impact to advocate for nurses and frontline staff, and help make decisions at a systems level.”
Romain chose Georgetown for her studies because the MHSA program combined a global health perspective with business and health care studies. She also appreciates the small class size and variety of backgrounds of her peers, who all contribute to classroom conversations based on their own experiences.
“As a nursing student, my classes were very clinically focused and I didn’t have the chance to take classes involving management strategy or reimbursement policy,” said Romain. “I’ve really enjoyed my classes and found the policy discussions so interesting to engage with.”
Romain opted to participate in the comparative health systems global experience for the past two years, visiting both Brazil and South Korea to study their health systems.
“I’ve learned that even though other countries’ health systems look different, we still struggle with similar issues, like workforce shortages and rural health care access,” said Romain. “The main difference is that we are a multipayer system, whereas both Brazil and South Korea have single-payer systems. With this, we see drastic differences in health care delivery costs. The U.S. is often looked up to for its diversity and complexity of care delivery, while we often admire other countries’ cost-containment methods.”
After graduating this month, Romain will start an administrative fellowship with Inova, based in northern Virginia. As part of her yearlong fellowship, she will rotate through various administrative departments in the hospital system, including finance, supply chain and managerial staff.
Studying the Intersection of Law and Health Care
While in law school two years ago, Thomas Levu (G’24) became interested in learning more about the intersection of law and health care.

Thomas Levu (G’24)
“In my law clinic, I worked with clients who were denied health coverage and health services,” said Levu. “I worked with clients to learn what legal remedies they had in accessing services and learned so much about how our health care system in the United States works by doing so.”
Levu was drawn to Georgetown to pursue his MHSA degree in part because of the program’s focus on experiential learning. He was awarded the Commission of Accreditation of Healthcare Management Education (CAHME)/Judy Baar Topinka Scholarship for Health Policy during his first year of the program. The scholarship recognizes a graduate student focusing on health policy who exemplifies hard work, ethical leadership and perseverance.
“I attended the national CAHME conference to receive the award, where I learned a lot about different innovations in health care,” said Levu. While the conference is mainly attended by health care executives, he noted that Christopher King, PhD, MHsc, FACHE, dean of the School of Health, was there and connected with Levu.
The class that stuck with Levu from his MHSA studies was a financial management course that pushed students to consider what they could accomplish with limited financial resources. “We were thinking through how far a hospital system could push their financial limits to serve the community with health care needs,” said Levu.
For his MHSA capstone research project, Levu circled back to his interest in law and health care by creating a uniform guide for hospitals and health care systems to implement medical-legal partnerships. As part of his research, Levu conducted interviews with individuals involved with medical-legal partnerships from Georgetown’s Health Justice Alliance, Whitman-Walker and the Suffolk Health Law Clinic.
“A patient could be presenting with a chronic respiratory illness and a physician realizes that the condition can’t really be addressed unless a mold issue in a person’s home is fixed,” said Levu. “There’s a good amount of research that shows once access to social benefits like housing are cut off, it leads to a person to seek more health care services. A legal remedy could exist that could help the person’s health.”
Levu presented his work on medical-legal partnerships in April to administrators at the Children’s National Hospital in Washington, DC. He hopes to work as in-house counsel for a health care system after graduation.
Improving Care, Improving Access
Madison Harbin (G’25), who is in her first year of the MHSA program, knew she always wanted to work in health care. She started working at a pharmacy in high school and also worked as a patient care tech at a local hospital while pursuing her undergraduate degree in health care management.

Madison Harbin (G’24)
“I was interested in trying to understand the patient side of care as well as learning about hospital operations during my time in undergrad,” said Harbin. One day after graduation, Harbin stumbled across an article on LinkedIn by King and told her parents she wanted to study at Georgetown.
“Dean King focuses on health equity and community needs,” said Harbin. “Listening to him and learning about caring for the whole person really showed how Georgetown was different from other schools.”
Harbin realized she needed more work experience in the health care sector before enrolling at Georgetown, so she worked first as a community outreach liaison at a hospital in Austin, Texas, and then as an executive focused on corporate relations with Healthcare Information and Management Systems Society (HIMSS) based in Asheville, North Carolina.
Since starting the MHSA program last fall, Harbin has enjoyed meeting her classmates and learning about their varied backgrounds. “I’m glad Georgetown brings all of us together with different work experiences,” she said. “I enjoy hearing their input, because it makes me think in a different way — like hearing my classmate who worked in a clinical setting bring up something related to patient care and Medicare, which I wouldn’t have thought of initially.”
Harbin’s favorite class to date has been operations management. She is preparing to focus her capstone research project for the class on rural health care in the United States.
“I grew up in a small town in Alabama, where we had to drive an hour and half to find care for my grandfather after he experienced a stroke,” said Harbin. “I’m interested in learning about expanding access to health care, especially for stroke patients, in rural areas, possibly through the use of telemedicine.”
Heather Wilpone-Welborn
GUMC Communications